March 5 is Dissociative Identity Disorder (DID) Awareness Day. We turned to EMDRIA member Jamie Marich, Ph.D., to help us understand more about EMDR therapy and Dissociative Identity Disorder (DID).
EMDR Therapy and Dissociative Identity Disorder (DID)
Guest Blog Post by Jamie Marich, Ph.D., LPCC-S, REAT, RYT-500 (she/they/we)
One of the most frequent questions that I receive in my role as an EMDR therapy trainer is whether people with dissociative experiences, specifically those with Dissociative Identity Disorder (DID), are appropriate for EMDR therapy. This question is such a hotly debated topic in the EMDR community. Many new EMDR therapists hear things like (a) my EMDR trainer told me never to let my clients dissociate, (b) If you give someone a DES and they score over 30, it’s a “rule out” for EMDR therapy, and (c) You can permanently damage someone with DID if you do EMDR with them. Many of these opinions come from a well-intentioned place of not wanting to do further harm to people with DID who’ve already been significantly traumatized. Yet sometimes that over-cautiousness can be harmful if that caution keeps us from offering folks with dissociative experiences the trauma processing help that they most need. When facing the question of whether a person with DID can handle EMDR therapy, the answer is not an easy yes/no. My short answer is yes, people with DID can be appropriate for EMDR therapy if the clinician offering the EMDR therapy is not afraid of dissociation. If a clinician is newly coming out of an EMDR training and they are terrified when a client even shows the first signs of dissociation in their office, of course, I wouldn’t want somebody with DID working with them until that clinician gets more training, more consultation and works on some of their hang-ups around their own personal dissociative experiences. Our hesitancy to look at our relationship with dissociation, something that we all do in the human experience, is what causes much of the fear.

Tell us a little bit about you, your experience becoming an EMDR therapist, and what drew you to the topic of dissociative identities.
My introduction to EMDR therapy came through seeking out help for my own dissociative experiences in 2004. I was two years into my addiction recovery journey and in graduate school for clinical mental health counseling. The internship site I served at was a constant source of activation as I saw children being mistreated by systems designed to help them. Dissociative symptoms and manifestations that were with me since childhood showed up in my life again after a period of sobriety, which I’ve come to learn is common for people in early recovery. Fortunately, a professor in my graduate program referred me to Janet Thornton, an early EMDR therapist in my hometown of Youngstown, Ohio. Janet accurately diagnosed me with Dissociative Disorder, NOS at the time (now Otherwise Specified Dissociative Disorder-1), and my whole work suddenly made sense. She was a prime model of an EMDR therapist who was not afraid of dissociation; rather, she worked with it, she navigated it, and she helped me—a dissociative system with many distinct parts—receive the life-changing power of EMDR therapy. I hope that one day, every person with dissociative experiences or diagnoses can have an EMDR therapist like I had with Janet.
How can EMDR therapy help clients who experience dissociation? And/Or What successes have you seen when using EMDR therapy with clients who identify as dissociative?
The word dissociation comes from a Latin root meaning to sever or divide. What do people sever or divide from when faced with traumatic or otherwise stressful experiences? Typically the present moment because it is unpleasant, painful or tortuous. And often those actively enduring trauma will not just daydream or stare off into space—the kind of dissociative behaviors to which all human beings are susceptible just by the nature of having to handle this thing we call life. Often, we will sever or divide parts or aspects of our experiences. Yes, sometimes this happens through developing distinct alters or parts that can help us hold pieces of the traumatic experience that are too much for any young person to carry. Keeping it very real, the severing of experience is not just about the development of parts. That severing can show up as the body-mind divide with which so many of our clients (and indeed, so many clinicians) struggle. If you’ve ever described yourself or a client as being “so in their head” or in the safety of logic and reason instead of letting themselves feel and notice the body, that is also a form of dissociation. So clearly, with these behaviors having roots in unhealed trauma, EMDR therapy could naturally prove helpful. As several people with dissociative experiences that I/we spoke to for my 2023 book Dissociation Made Simple: A Stigma-Free Guide to Embracing Your Dissociative Life and Navigating Life shared in their interviews, it’s not the dissociation that is the problem—the dissociation is an often adaptive response to trauma. The trauma and the damage caused by it is the problem. So why wouldn’t we engage one of the most powerful trauma processing methods available to us today, EMDR, to help?
Are there any cautionary measures you would like to mention regarding the use of EMDR therapy with clients who have a dissociative disorder?
Definitely—for EMDR therapy to be successfully used with dissociative disorders, modifications will need to be made based on the unique needs of the dissociative system presenting for care. This is another one of those questions where I cannot give you an easy answer because if you’ve met one dissociative system, you’ve met only one dissociative system. If you are stuck, get consultation. Consultation is even more valuable than training when first learning to work with EMDR and dissociative disorders because a skilled consultant can walk you through the intricacies of a specific person/system’s case. I will offer, in general, the following best practices: (a) The “Calm Safe Place” exercise that just about every EMDR therapy trainer shares based on Shapiro’s emphasis on the skill will not be sufficient for preparation. Indeed, most, if not all, dissociative systems already know how to go away in their mind to feel better, so skill focus in Phase 2 will need to be more on grounding, anchoring, or other skills that can help a person/system and their various parts stay present, (b) Like with many complex trauma cases, it’s typically best to start with present prong or current stressor targets instead of going back to touchstone memories immediately. Wherever possible, when I know that I’m working with a dissociative system, I attempt to get system consensus on where we start with targeting sequence work by asking a question like, “Where is their willingness to work today?” Even in a standard protocol set up, instead of asking for the image representing the worst part of a target memory, I will ask what part of any given memory a system is willing to work on today. It’s a modification, yes, yet in EMDR’s wisdom, the brain will take the processing where it needs to go and help the person/system get to where they need to work more gently. And of course, have your stop and pause signs at the ready and a plan for what to do should a person and/or one of their parts choose to take that pause. Be advised that different parts of a dissociative system may require different resources.
Any specific complexities folks with dissociative disorders might deal with that might impact EMDR therapy?
There are so many yet in an article of this length I can only focus on a few. The two that feel most important to share are that clients with dissociative experiences may need a little extra assistance in reprocessing instead of just the “Go with that” prompt that defines EMDR therapy. As one of my former clients shared with me, “When you said go with that, I always wanted to clap back with, ‘Go with what?’” Even though the conventional EMDR training ethic is to not repeat things for the client and to stay out of the way as much as possible, for clients that might dissociate or get thrown off balance more easily, I generally find that it’s okay for the therapist to talk more and to offer more in the way of interweaves or proactive measures if needed.
Also, the official precaution many trainers give on working with dissociation is to give a tool like the DES or the MID in advance to know what you’re dealing with. Although, as a clinician, I’m not opposed to using the DES. I teach this tool in my EMDR trainings; as a person with a dissociative disorder, I want to let you all in on an insider pro-tip: Many of us have systems that have a part that is used to hold it all together that may tell you exactly what you want to hear on those kinds of assessments. So you may think that you’re starting EMDR therapy with a client who doesn’t have a lot going on in the way of dissociative expression or even having a defined system. Then, the reprocessing may take you and your client both by surprise as parts emerge that have a great deal to say (or to protect) about what’s coming up in the EMDR. The great thing about the EMDR phases is that they are fluid—you can always retool and return to Phase 2, which may include more psychoeducation about dissociation and parts.
What multicultural considerations might EMDR therapists need to keep in mind regarding EMDR therapy and dissociative disorders?
We love this question, and thank you, EMDRIA, for asking it! Candidly, the idea of dissociation and parts as pathological constructs is the invention of Western psychology. When I engaged in the interviews for Dissociation Made Simple, I made a special effort to talk to a variety of traditional Shamans and Native American and Canadian folks who are steeped in these practices. Indeed, people with dissociative gifts who have a capacity to dance between their parts and listen to their wisdom are seen as the healers and the shamans in many global traditions. Wouldn’t it be great if we, as Western-trained therapists, could listen to the wisdom of parts and alters and honor the stories that they value instead of just writing them off as problematic? A major lesson I learned from one of the Shamans I interviewed, Julian Jaramillo from the Chocó people in Ecuador, is that in traditional Shamanism the brain, as we are so obsessed with in modern psychotherapy practice, doesn’t exist for the elders. Instead, his people speak about things in terms of feelings, sensations, stories, and symbols. As a dissociative mind and a qualitative thinker/researcher, the connection to mythology and story as avenues for helping people and systems heal is potent and far too overlooked in the Western medical model.
Also, as a practice in cultural humility with dissociative disorders or any other diagnosis, we encourage you to listen to your clients. There is a real Pride movement happening in the community of people with dissociative disorders and experiences in recent years. We’ve adopted the anthem that rings through many other marginalized communities: nothing about us without us. Largely, we are frustrated with the way that many professionals researching or even teaching dissociation without their own lived experiences of dissociative disorders are representing us. This reality is a major reason that I decided to come out in 2018 fully. If a client with a dissociative system wants to explore a new way of doing things within EMDR therapy, be willing to talk it at least out, and likely following their lead will be best. I still cringe every time dissociative systems report to me, “Well, my EMDR therapist won’t talk to my parts directly because they had a trainer tell them not to.” Listen to your clients, and be willing to, as several contributors to Dissociative Made Simple shared with me, “throw out your textbook.”
What is your favorite free resource to suggest to other EMDR therapists working with this population?
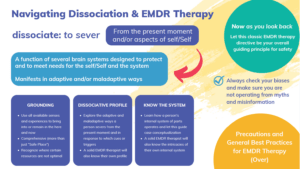
Everything that I’ve/we’ve done for free online can be accessed at: https://redefinetherapy.com/press-media-resources/. This site includes every podcast interview I’ve done on dissociation and many free articles and resources. My training group, the Institute for Creative Mindfulness, also makes the resources page free for EMDR Therapists. You might especially be interested in the Dissociation Infographic downloadable PDF on that site that features my best practices for working with dissociative systems; it’s essentially an expanded answer to what we offered in Question #3.
“A quality therapeutic experience requires a fusion between solid relational skills and appropriate implementation of clinical techniques.” (Marich, 2023, p. 232)
“Listen to [clients] feedback about whether a certain approach you are trying with EMDR is working, and be willing to adapt. Flexibility and adaptability are, without a doubt, two of the most important traits you can have when working with any clients.” (Marich, 2011, p. 282)
 Dr. Jamie Marich (she/they) is an EMDRIA Certified Therapist, Trainer and Consultant. She is a TEDx speaker, clinical trauma specialist, expressive artist, lay spiritual director, short filmmaker, Reiki master, yoga teacher, and recovery advocate, and unites all of these elements in her mission to redefine therapy. She is a woman in long-term recovery from an addictive disorder and lives with dissociative identities.
Dr. Jamie Marich (she/they) is an EMDRIA Certified Therapist, Trainer and Consultant. She is a TEDx speaker, clinical trauma specialist, expressive artist, lay spiritual director, short filmmaker, Reiki master, yoga teacher, and recovery advocate, and unites all of these elements in her mission to redefine therapy. She is a woman in long-term recovery from an addictive disorder and lives with dissociative identities.
Marich teaches topics related to trauma, EMDR therapy, expressive arts, and spiritual abuse while maintaining a private practice and online education operations in her home base of Akron, Ohio. Marich founded the Institute for Creative Mindfulness and developed the Dancing Mindfulness approach to expressive arts therapy.
Marich is the author of several books, most recently Dissociation Made Simple: A Stigma-Free Guide to Embracing Your Dissociative Mind and Navigating Life (2023) and Trauma and the 12 Steps: The Workbook (with Stephen Dansiger, 2023). Her long-time publisher, North Atlantic Books, is releasing her memoir of spiritual abuse and recovery, You Lied to Me About God, in October 2024.
References
EMDRIA. EMDR therapy and dissociative disorders with Dr. Jamie Marich. Let’s Talk EMDR. https://www.emdria.org/podcast/emdr-therapy-and-dissociative-disorders/
Marich, J. (2023). Dissociation Made Simple (p.232). Berkeley, CA: North Atlantic Books
Marich, J. (2011) EMDR Made Simple (p. 282). Eau Claire, WI: Premier Publishing & Media.
Back to Focal Point Blog Homepage
Additional Resources
If you are a therapist interested in the EMDR training:
- Learn more about EMDR at the EMDRIA Library
- Learn more about EMDR Training
- Search for an EMDR Training Provider
- Check out our EMDR Training FAQ
If you are EMDR trained:
- Check out EMDRIA’s Let’s Talk EMDR Podcast
- Check out the EMDRIA blog, Focal Point
- Learn more about EMDRIA membership
- Search for Continuing Education opportunities
If you are an EMDRIA Member:
- Learn more about EMDR Consultation
- Find clinical practice articles in EMDRIA’s Go With That Magazine
- Search for articles in Journal of EMDR Practice and Research in the EMDRIA Library
Date
March 4, 2024
Contributor(s)
Jamie Marich
Topics
Dissociation





