*This blog post was updated from an original post published June 2021*
June is PTSD Awareness Month. PTSD stands for posttraumatic stress disorder, a condition that some people experience after one or several traumatic events. EMDR therapy is shown to be one of the most effective treatments for PTSD. Common questions we receive about PTSD are:
- What is trauma?
- When does the experience of trauma cross the threshold into becoming PTSD?
- How does EMDR therapy help PTSD?
What is Trauma?
Trauma is an event or experience of an event that overwhelms our ability to make sense of what is happening to us. Trauma affects many people. In a 2015 worldwide survey “over 70% of respondents reported a traumatic event” such as accidental injury, physical/sexual assault, an unexpected family death, or being robbed (Benjet et al., 2015).
Bessel van der Kolk (2014) highlighted the prevalence of trauma in the introduction of his bestselling book on trauma, The Body Keeps the Score. He referenced the groundbreaking Felitti et al., (1998) study on the link between childhood trauma and negative health consequences later in life. Childhood trauma is referred to as Adverse Childhood Events or ACEs in the study. 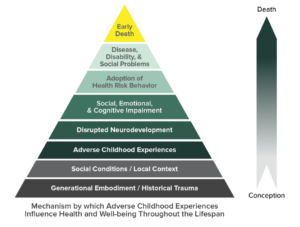 “Research by the Centers for Disease Control and Prevention has shown that one in five Americans was sexually molested as a child; one in four was beaten by a parent to the point of a mark being left on their body, and one in three couples engages in physical violence. A quarter of us grew up with alcoholic relatives, and one out of eight witnessed their mother being beaten or hit” (van der Kolk, 2014).
“Research by the Centers for Disease Control and Prevention has shown that one in five Americans was sexually molested as a child; one in four was beaten by a parent to the point of a mark being left on their body, and one in three couples engages in physical violence. A quarter of us grew up with alcoholic relatives, and one out of eight witnessed their mother being beaten or hit” (van der Kolk, 2014).
During a traumatic event, the danger or perceived danger disconnects us from the moment, from our reactions, or from others. Our brains and nervous systems react automatically to protect us. This reaction is the fight, flight, or freeze response. This response prompts our bodies to go into survival mode by increasing heart rate, releasing stress hormones, and increasing blood flow to prepare for running or protecting. Certain parts of the brain are also affected, including the amygdala, the hippocampus, and the prefrontal cortex. The amygdala acts as the emotional alarm of the brain when we feel unsafe. When activated by trauma, it may disrupt signals to the hippocampus, which is important for long-term memory storage. This is why trauma memories may seem fragmented. The prefrontal cortex, which monitors rational thought and helps us control emotional responses, may go off-line when the amygdala signals the need for alarm. ‘Thinking your way’ out of the situation is much more difficult, and is why trauma reactions may not always seem logical. Trauma memories are often associated with images, feelings, and body sensations, rather than rational thoughts.
What is PTSD?
Posttraumatic stress disorder (PTSD) refers to a specific set of criteria regarding trauma symptoms in the DSM-5. The DSM-5 is the handbook most health care professionals in the U.S. use to diagnose mental health issues. PTSD occurs when the symptoms and reactions caused by a traumatic event do not resolve in a few months. Someone who does not develop PTSD will be able to process, or make sense of the event and feel okay with moving on after the experience. Someone who does develop PTSD is so overwhelmed by the event that it does not resolve, remaining stored in the brain and nervous system in an unhealthy way. The memory lingers and disrupts everyday life. Sometimes one single trauma event (ie. natural disaster, car accident) can cause PTSD. Sometimes repeated events from childhood or ongoing traumatic events can create conditions for PTSD. The key is that the body and brain’s ability to cope is disrupted and overwhelmed.
PTSD symptoms generally fall into four areas:
- Re-living symptoms: flashbacks or nightmares.
- Avoidance symptoms: staying away from activities, people, or places that are reminders of the trauma.
- Cognition and mood symptoms: negative thoughts about self and world, extreme guilt, or lack of interest in things that used to be enjoyed.
- Increased arousal symptoms: startling easily, having angry outbursts, and difficulty sleeping.
Early research conducted on traumatic experiences that led to PTSD focused mainly on combat-related traumatic experiences in primarily male samples (National Center for PTSD). As the field expanded, gender-based differences in traumatic experiences are showing up in the research, showing that “more than half of all women will be exposed to at least one traumatic event in their lifetime” and the type of traumatic events women experience are more frequently interpersonal such as sexual assault – one of the highest risk factors for PTSD. (American Psychological Association, 2023). PTSD Alliance reported that 70% of adults in the U. S. have experienced at least one traumatic life event and that 20% of those people may develop PTSD. In addition, they showed how the risk of developing PTSD can vary depending on the trauma experienced. The National Center for PTSD states that “PTSD can happen to anyone. It is not a sign of weakness.” Populations at higher risk for developing PTSD are enlisted military (especially those who have been in active-duty combat), rape victims, refugees and asylum seekers, child abuse victims, first responders, sexual assault victims, LGBTQ+, especially transgender individuals, those in war zones, and those who have been physically attacked.
EMDR Therapy for PTSD
EMDR therapy is one of several psychotherapies available for the treatment of PTSD. It has proven effective for the treatment of PTSD in research and in clinical practice. De Jongh, et al. (2019) wrote about this efficacy and evidence base in the article “The Status of EMDR Therapy in the Treatment of Posttraumatic Stress Disorder 30 Years After Its Introduction.” EMDR therapy has been recognized as effective for PTSD in the treatment guidelines of national and international organizations. These organizations include the International Society for Traumatic Stress Studies, the U.S. Department of Veterans Affairs, and the World Health Organization. The assessments and recommendations of these organizations are based on decades of clinical research. EMDR therapy is also becoming recognized as one of the most cost-effective treatments for PTSD.
EMDR therapy has been recognized as effective for PTSD in the treatment guidelines of national and international organizations. These organizations include the International Society for Traumatic Stress Studies, the U.S. Department of Veterans Affairs, and the World Health Organization. The assessments and recommendations of these organizations are based on decades of clinical research. EMDR therapy is also becoming recognized as one of the most cost-effective treatments for PTSD.
Dr. Judith Herman notes three stages in trauma recovery: “establishing safety, retelling the story of the traumatic event, and reconnecting with others… [and] ordinary life.” EMDR therapy covers all three of these stages throughout the 8 phases of treatment. One aspect of EMDR therapy that many clients appreciate is that the retelling of the traumatic event does not have to be verbal. Instead of talking about the trauma, the client is asked to bring aspects of the trauma memory to mind such as an image, cognition, emotion, and body sensation. While doing this, the EMDR therapist keeps the client in the present moment with alternating eye movements, sounds, or taps. The alternating eye movements, sounds, or taps are another part of treatment that sets EMDR therapy apart: they are referred to as dual attention stimulus (DAS) or bilateral stimulation (BLS). As with other trauma therapies, the EMDR therapist guides the therapy process with the goal of keeping the client feeling safe. The client has full control to stop the therapist at any point if needed. Clients who have had success with EMDR therapy often experience positive shifts in insight regarding their trauma experience. They no longer feel overwhelmed by the trauma.
EMDR therapy for PTSD treatment is not only established in research-based treatment guidelines but also becoming mainstream. The organization PTSD UK showcases several personal experiences using EMDR therapy for PTSD. Recent headlines for EMDR therapy discussed Prince Harry being filmed in an EMDR therapy session in the Apple+ TV documentary The Me You Can’t See. Other celebrities such as Sandra Bullock, Lady Gaga, Jameela Jamil, Evan Rachel Wood, and more have also reported success with EMDR therapy.
If you have PTSD and are interested in EMDR therapy, the EMDRIA website has a directory in which you can search for EMDR therapists near you.
Susanna Kaufman, M.A., works with content at EMDRIA, compiling and editing Focal Point blog posts while working toward her full LPC licensure in Texas.
Resources
American Psychological Association. What is EMDR therapy and why is it used to treat PTSD? www.apa.org/topics/psychotherapy/emdr-therapy-ptsd
American Psychological Association. Women who experience trauma are twice as likely as men to develop PTSD. Here’s Why. www.apa.org/topics/women-girls/women-trauma
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., Shahly, V., Stein, D. J., Petukhova, M., Hill, E., Alonso, J., Atwoli, L., Bunting, B., Bruffaerts, R., Caldas-de-Almeida, J. M., de Girolamo, G., Florescu, S., Gureje, O., Huang, Y., … & Koenen, K. C. (2016). The epidemiology of traumatic event exposure worldwide: Results from the World Mental Health Survey Consortium. Psychological Medicine, 46(2), 327-343. Open access: https://doi.org/10.1017/S0033291715001981
Brainfacts.org. 3D Brain. www.brainfacts.org/3d-brain#intro=false&focus=Brain
Centers for Disease Control and Prevention. About the CDC-Kaiser ACE study [Image]. www.cdc.gov/violenceprevention/aces/about.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fviolenceprevention%2Facestudy%2Fabout.html
Centers for Disease Control and Prevention. Adverse Childhood Experiences (ACEs): Preventing early trauma to improve adult health. www.cdc.gov/vitalsigns/aces/index.html
de Jongh, A., Amann, B. L., Hofmann, A., Farrell, D., & Lee, C. W. (2019). The status of EMDR therapy in the treatment of posttraumatic stress disorder 30 years after its introduction. Journal of EMDR Practice & Research, 13(4), 261-269. Open access: https://doi.org/10.1891/1933-3196.13.4.261
EMDRIA. EMDR therapy and PTSD. www.emdria.org/about-emdr-therapy/emdr-ptsd/
EMDRIA. EMDR therapy gains celebrity exposure. www.emdria.org/blog/emdr-therapy-gains-celebrity-exposure/
EMDRIA. EMDR therapy in treatment guidelines. www.emdria.org/about-emdr-therapy/emdr-and-ptsd/
EMDRIA. The eight phases of EMDR therapy. www.emdria.org/blog/the-eight-phases-of-emdr-therapy/
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., Koss, M. P., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventative Medicine, 14(4), 245-258. Open access: https://doi.org/10.1016/S0749-3797(98)00017-8
Herman, J. (2002). Recovery from psychological trauma. Psychiatry and Clinical Neurosciences, 52(S1), S98-S103. Open access: https://doi.org/10.1046/j.1440-1819.1998.0520s5S145.x
Livingston, N. A., Berke, D., Scholl, J., Ruben, M., & Shipherd, J. C. (2020). Addressing diversity in PTSD treatment: Clinical considerations and guidance for the treatment of PTSD in LGBTQ populations. Current Treatment Options in Psychiatry, 7(1), 53-69. Open access: https://doi.org/10.1007%2Fs40501-020-00204-0
Macleod, M. (2021). PTSD may be more common than we think. How do you know if you have it? Get the Gloss. www.getthegloss.com/health/mental-health/what-is-ptsd-and-how-to-mange-symptoms
Mavranezouli, I., Megnin-Viggars, O., Grey, N., Bhutani, G., Leach, J. Daly, C., Dias, S., Welton, N. J., Katona, C., El-Leithy, S., Greenberg, N., Stockton, S., & Pilling, S. (2020). Cost-effectiveness of psychological treatments for post-traumatic stress disorder in adults. PLoS ONE 15(4): e0232245. Open access: https://doi.org/10.1371/journal.pone.0232245
Maxfield, L. (2019). Editorial: A clinician’s guide to the efficacy of EMDR therapy. Journal of EMDR Practice & Research, 13(4), 239-246. Open access: https://doi.org/10.1891/1933-3196.13.4.239
National Center for PTSD. How common is PTSD in adults? www.ptsd.va.gov/understand/common/common_adults.asp
National Center for PTSD. Research on women, trauma, and PTSD. www.ptsd.va.gov/professional/treat/specific/ptsd_research_women.asp
National Institute of Mental Health. Post-traumatic stress disorder. www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
SAMHSA. (2014) Trauma-Informed Care in Behavioral Health Services (Treatment Improvement Protocol TIP Series, No. 57). Exhibit 1.3-4, DSM-5 Diagnostic Criteria for PTSD. www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16/ Taken from: American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association.
PsychCentral. Can you recover from Trauma? 5 therapy options. https://psychcentral.com/health/trauma-therapy
PTSD Alliance. What is posttraumatic stress disorder. www.ptsdalliance.org/about-ptsd/
SOL Mental Health. (2021, Sept 15). The crucial relationship between PTSD and the body. Psychology Today. www.psychologytoday.com/us/blog/psychiatry-the-people/202109/the-crucial-relationship-between-ptsd-and-the-body
Turrini, G., Tedeschi, F., Cuijpers, P., Del Giovane, C., Kip, A., Morina, N., Nose, M., Ostuzzi, G., Purgato, M., Ricciardi, C., Sijbrandij, M., Tol, W., & Barbui, C. (2021). A network meta-analysis of psychosocial interventions for refugees and asylum seekers with PTSD. BMJ Global Health, 6:e005029. Open access: https://doi.org/10.1136/bmjgh-2021-005029
U.S. Department of Veterans Affairs. Help raise PTSD awareness. www.ptsd.va.gov/understand/awareness/index.asp
van der Kolk, B. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. New York, NY: Penguin Books
Back to Focal Point Blog Homepage
Additional Resources
If you are a therapist interested in the EMDR training:
- Learn more about EMDR at the EMDRIA Library
- Learn more about EMDR Training
- Search for an EMDR Training Provider
- Check out our EMDR Training FAQ
If you are EMDR trained:
- Check out EMDRIA’s Let’s Talk EMDR Podcast
- Check out the EMDRIA blog, Focal Point
- Learn more about EMDRIA membership
- Search for Continuing Education opportunities
If you are an EMDRIA Member:
Date
June 14, 2024
Contributor(s)
Susanna Kaufman
Topics
PTSD